Airway Clearance Therapy for NTM Patients
Benefits of Airway Clearance Therapy in Patients with Non-Tuberculous Mycobacteria (NTM)
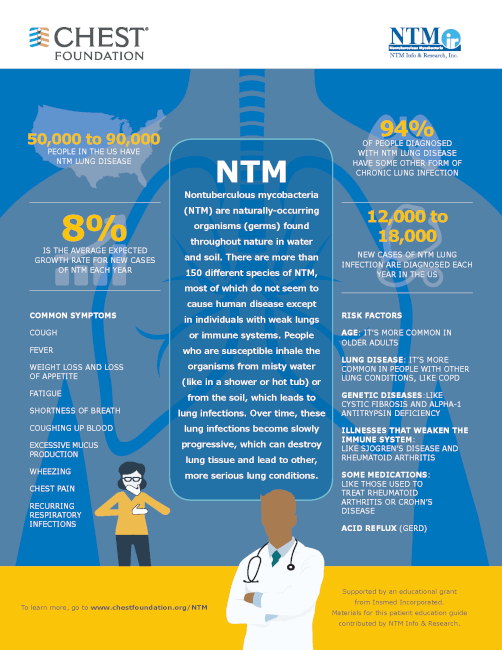
Nontuberculous mycobacterial (NTM) is an infection caused by bacteria that is inhaled in through the nose and mouth. NTM bacteria are common in the everyday environment and can be found in places such as common water sources and soil. It is estimated that approximately 170,000 people in the United States have NTM lung disease, and 12,000 to 18,000 people become infected each year. The rate of infection increases significantly in populations over the age of 65. NTM typically develops in people with preexisting lung conditions such as bronchiectasis, COPD, and asthma.
Symptoms of NTM
NTM can cause symptoms such as coughing, fatigue, and shortness of breath. Over time symptoms can worsen, because NTM is progressive. The infection can get worse over time and can result in severe, permanent lung damage if not treated properly.
Symptoms of NTM lung disease can be classified into two categories: symptoms that mainly affect the lungs and symptoms that affect the whole body.
The most common respiratory symptoms of NTM lung disease are:
- Persistent cough
- Coughing up blood
- Shortness of breath
Other symptoms of NTM lung disease include:
- Fatigue
- Low-grade fever
- Night sweats
- Weight loss
Diagnosing NTM
A chest X-ray may provide the first hint that NTM are present. However, a CT scan is required to show more detail that can help confirm NTM. The CT scan can show the presence of small nodules in the lungs and identify cavities or holes in the lung, which represent a more destructive form of infection. The conclusive diagnosis of NTM infection is done through a culture of mucus. In some cases, where mucus cannot be not produced, a bronchoscopy is performed to obtain the sample.

Treatment Options for NTM
Once diagnosed, there are several options in treating NTM. Antibiotics are vital in treating NTM. However, many NTM bacteria have some natural resistance to certain antibiotics, and NTMs can easily develop resistance. Typically, the treatment regimen includes combination antibiotic therapy. To overcome drug resistance, people with NTM may need to take several different antibiotics at the same time. Because these medications may have side effects, close monitoring is important. The goal of treatment is to achieve negative mucus cultures and maintain that for 12 months before stopping. Sometimes treatment is ongoing, depending on the severity of the disease. In addition to antibiotic treatment of the infection, it is important to address airway clearance in NTM lung diseases.
Airway Clearance Therapy for NTM
Airway clearance should be an integral part of any treatment plan for NTM lung disease. When mucus sits in your airways, it causes inflammation and possibly further damage to your lungs. Mucus also holds bacteria in the airways, leading to more inflammation and recurrent exacerbations. Because of this, it is critical to improve airway clearance to get the mucus out of the airways. There are several airway clearance techniques that can be done to help treat individuals with NTM infection. Airway clearance therapy helps to expel mucus from the lungs using techniques such as nebulized hypertonic saline, manual chest physical therapy, oscillating devices, high frequency chest wall oscillation (HFCWO) therapy vests, huff coughing to help bring up mucus and increased aerobic exercise.

Mobile HFCWO therapy vests like the AffloVest can help with improvement in coughing up mucus, selected measures of lung function, and health-related quality of life. Mobile HFCWO therapy vests are typically worn for 20 to 30 minutes per day and provide percussion and vibration directly to the torso, targeting the upper and lower lobes of the lungs, to help loosen and thin the mucus off of airway walls and move them into the larger airways to be coughed up. The AffloVest can be worn in conjunction with other therapies such as nebulizing or performing postural drainage to increase mucus movement. Combining therapies should always be discussed with your care team.